Antimicrobial resistance (AMR) is an increasing global concern in small animal veterinary practices. The overuse and misuse of antimicrobials in companion animals can contribute to the spread of AMR between animals and humans. This study aimed to assess small animal veterinarians’ knowledge, attitudes, and behaviors towards antimicrobial use (AMU) and AMR in North Macedonia. A web-based questionnaire was developed, including questions addressing demographics, owner influence on antibiotic prescription and prescribing practices. The response rate of the small animal veterinarians was 47.50% (57/120), with most of them (84.20%) having 1-15 years of work experience. Pearson’s chi-square test of independence was used for contingency tables that met the chi-square assumption, and Fisher’s exact test was conducted for contingency tables that did not. Most veterinarians responded that they had perceived pressure and direct demands from pet owners to prescribe antimicrobials (35.09% frequently, 45.61% occasionally). In the survey, 50.77% of the veterinarians reported frequently administering antibiotics without conducting bacteriological or antimicrobial susceptibility testing. They typically resorted to these tests in cases with recurrent infections, such as skin infections (19.63%), or when empirical therapy is ineffective (14.72%). Based on the findings, it can be concluded that veterinarians play a crucial role in tackling the AMR in North Macedonia. The lack of stewardship programs or guidelines for responsible antimicrobial use in companion animals is a critical issue that requires urgent attention, emphasizing the vital role of veterinarians in combating AMR.
Antimicrobial resistance (AMR) is becoming a primary concern in small animal practices (
1). The overuse and misuse of antimicrobials significantly contribute to the spread of resistant bacteria and resistance genes between animals and humans (
2). The antimicrobial use (AMU) in companion animals is often overlooked as a contributing factor to the global AMR challenge, representing a significant gap in the One Health strategy for AMR surveillance (
3, 4). Over the past decade, multidrug-resistant (MDR) bacteria have emerged and spread among companion animals worldwide, with the potential for zoonotic transmission (
5). The most concerning MDR bacteria isolated in companion animals include methicillin-resistant
Staphylococcus spp., vancomycin resistant enterococci, extended-spectrum beta-lactamase (ESBL), AmpC and carbapenemase-producing Gram-negative bacteria (
6, 7, 8). All these bacteria have shown resistance to all licensed antimicrobials for animal use, posing a significant threat to animal health by increasing the risk of treatment failure (
9).
However, antimicrobial prescribing patterns are highly relevant to the efforts towards controlling AMR, which is an increasingly concerning issue in small animal practice (
10). In this context, critically important antimicrobials (CIAs), typically reserved for human medicine, are allowed within veterinary clinics (
11). Interestingly, it appears that CIAs are used more frequently in companion animals than farm animals despite the overall antimicrobial use being lower in companion animals (
12, 13). Therefore, the European Medicines Agency (EMA) has categorized antimicrobials into four groups based on their impact on public health and the need for use in veterinary medicine. Categories D and C should be used cautiously, whereas Categories B and A should be restricted or not being used in veterinary medicine (
12, 14). It is crucial to evaluate the use of these drugs in companion animals due to their impact on public health (
9, 10).
Recently, there has been an increasing emphasis worldwide on promoting responsible prescribing practices and reducing the use of antimicrobials in veterinary medicine (
7). Antimicrobial stewardship, as defined by the American Veterinary Medical Association (AVMA), is the responsibility of veterinarians to ensure the accessibility and effectiveness of antimicrobials while protecting animal, public, and environmental health (
15). Several European countries, including the Czech Republic, Denmark, Finland, France, Germany, Ireland, the Netherlands, Norway, Sweden, and the United Kingdom, have established surveillance programs to monitor AMR in animals. Some of these programs also include specific control measures and antimicrobial stewardship guidelines (ASGs) in animals, including companion animals (
16). Twelve European ASGs include statements to reserve high priority-CIAs (HP-CIAs) such as carbapenems and vancomycin exclusively for humans (
7). This is to raise awareness among practitioners who may not fully understand the importance of these drugs in combating AMR and the role of protecting public health.
No data is available on the usage of antimicrobials in companion animals treated in veterinary practices in North Macedonia. The antimicrobial resistance of the bacteria isolated from these species has not been thoroughly researched, except for the study of Cvetkovikj et al. (
17) which focused on AMR in clinical isolates of
Staphylococcus spp. in dogs in North Macedonia. Moreover, the lack of stewardship programs and guidelines for prudent antimicrobial use in companion animals is a serious concern that must be addressed. For this reason, understanding current antimicrobial prescribing practices is crucial for developing accurate stewardship strategies (
18). This study is a starting point for developing guidelines for antimicrobial use in companion animals in North Macedonia and presents the findings of a survey conducted among small animal veterinarians. The primary goal was to evaluate the veterinarians’ knowledge, attitudes and behaviors towards AMU and AMR in companion animals.
MATERIAL AND METHODS A survey was conducted to investigate the antimicrobial usage patterns among veterinarians who work in small animal practices. A questionnaire was designed and tested on ten small animal clinicians to evaluate its utility and identify potential issues. The pilot study was successful, and no changes were made to the questionnaire. The questionnaire and a cover letter detailing the study’s purpose were sent to 120 small animal veterinarians. The qualified participants received an email containing a link to the web-based questionnaire that was accessible for two weeks. The survey had five parts: demographics, owner influence on antibiotic prescription, prescribing practices and behavior, surgical prescribing practices, and antibiotics for specific/ systemic infections. It consisted of 19 questions focused on the veterinarians’ demographics, experiences in practice, current prescribing habits, individual opinions about antimicrobial usage, and bacteriological testing. The questionnaire offered a comprehensive overview of the antibiotics that small animal veterinarians may prescribe for various health conditions of the patients.
StatisticsFisher exact test was performed for contingency tables that were not fulfilling the chi-square assumption for cell counts n<5. Pearson’s chi square test of independence was performed for the other contingency tables that fulfilled this assumption. The significance level was set at p<0.05. The level of association for the positive responses of each question and the respective response categories was assessed with Cramer V value and the corresponding degrees of freedom (df). All responses were expressed as counts (n) and percentages (%).
RESULTS
Sociodemographic data of the survey participants
In total, 47.50% (57/120) of the invited veterinarians agreed to participate in the study and filled in the questionnaires providing information on AMU and AMR in North Macedonia. Most veterinarians were male, 57.89% (33/57), while 93% (53/57) were in the age category <50 years.
There was no significant difference in the gender of the participants. They were mainly in the age range between 25-30 years (n=31, 54.39%) and 36-50 years (n=22, 38.60%). The association level of these age groups with the acceptance to participate in the survey was high (V=0.42, df=2). A significantly higher number of participants (n=54, 83.08%) had between 1 and 15 years of work experience. This was highly associated with the acceptance to participate in the survey (V=0.75, df=2).
Table 1 depicts the sociodemographic data distribution.
 The influence of pet owners on the antibiotic prescription practice of veterinarians
The influence of pet owners on the antibiotic prescription practice of veterinariansA significantly higher number of veterinarians answered that pet owners occasionally (n=31, 54.39%) or frequently (n=22, 38.61%) give antibiotic therapy before seeking professional veterinary care compared to responses as ‘always’ (n=3, 5.26%) and 'never’ (n=1, 1.75%). The level of association was high (V=0.51, df=3).
A significantly higher number of veterinarians answered that pet owners occasionally (n=26, 45.61%) or frequently (n=20, 35.09%) request antibiotic treatment for their pets compared to those who responded ‘always’ (n=8, 14.04%) and ‘never’ (n=3, 5.26%). The level of association was high (V=0.38, df=3).
The highest number (n=34, 59.65%) of veterinarians answered that pet owners occasionally demand bacteriological testing. The number of veterinarians (n=22, 38.60%) who answered that pet owners have never demanded this type of testing was significantly lower compared to the previous group of veterinarians, but still significantly higher compared to the veterinarians who have responded “frequently” (n=1, 1.75%). There were no answers with “always.” The level of association was high (V=0.38, df=3).
The detailed distribution of the responses is shown in
Table 2.
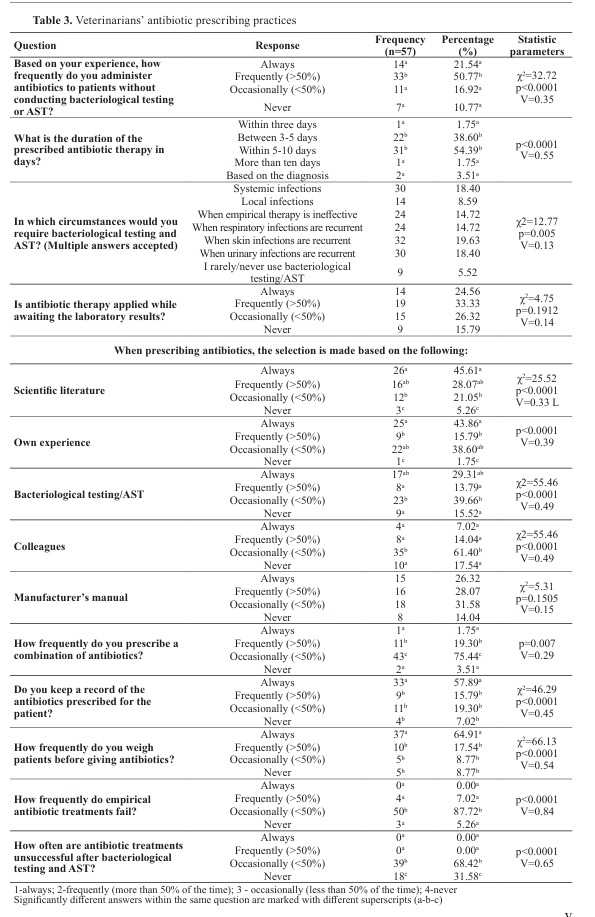
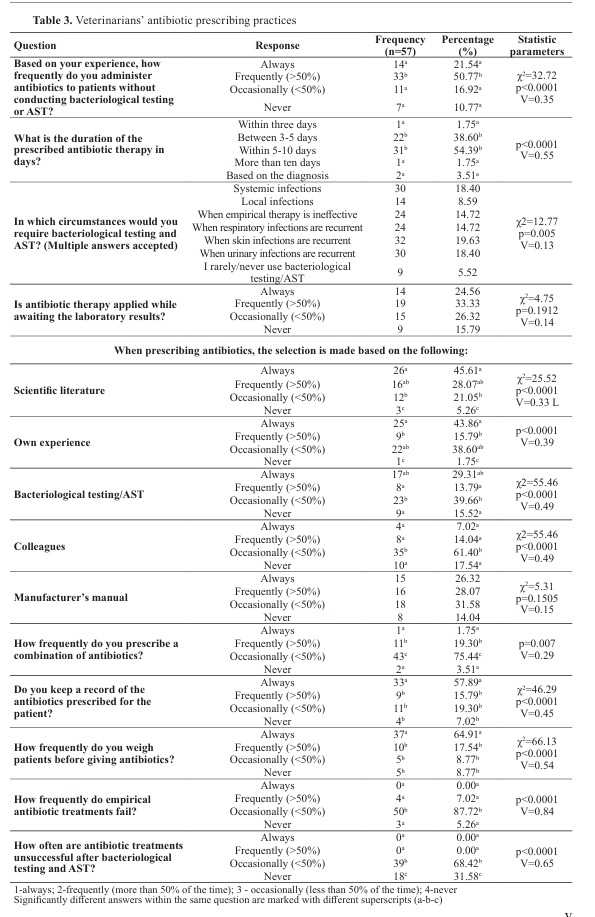
 Veterinarians’ antibiotic prescribing practices
Veterinarians’ antibiotic prescribing practicesA significantly higher number of veterinarians (n=33, 50.77%) have declared that they frequently administer antibiotics without conducting bacteriological testing or AST compared to veterinarians answering ‘always’ (n=14, 21.54%), ‘occasionally’ (n=11, 16.92%), and ‘never’ (n=7, 10.77%). The level of association was high (χ2=32.72, V=0.35, df=3).
A significantly higher number of veterinarians have declared that the duration of the prescribed antibiotic therapy was between 3-5 days (n=22, 38.60%) and within 5-10 days (n=31, 54.39%), compared to veterinarians answering ‘based on the diagnosis’ (n=2, 3.51%), ‘within three days’ (n=1, 1.75%), and ‘more than ten days’ (n=1, 1.75). The level of association was high (V=0.55, df=4).
Most of the veterinarians have answered that they require bacteriological testing and AST in recurrent skin infections (n=32, 19.63%), systemic infections (n=30, 18.40%), recurrent urinary infections (n=30, 18.40%), ineffective empirical therapy (n=24, 14.72%), and recurrent respiratory infections (n=24, 14.72%). They were non significantly different (χ2=12.77, V=0.13, df=6) and the level of association was medium.
There was no significant difference in the responses regarding how often the antibiotic therapy was applied while awaiting the laboratory results. They ranged between 15.79% (n=9) for ‘never’ and 33.33% (n=19) for ‘frequently’. The level of association was low (χ2=4.75, V=0.14, df=3).
The antibiotic therapy selection based on the scientific literature was used ‘always’ (n=26, 45.61%) and ‘frequently’ (n=16, 28.07%) by a significantly higher number of veterinarians. A significantly lower number of veterinarians answered ‘occasionally’ (n=12, 21.05%) and ‘never’ (n=3, 5.26%). The association level was high (χ2=25.52, V=0.33, df=3).
The antibiotic therapy selection based on own experience was answered ‘always’ (n=25, 43.86%) and ‘occasionally’ (n=22, 38.60%) in significantly high number of veterinarians. The response for ‘frequently’ (n=9, 15.79%) and ‘never’ (n=1, 1.75%) was given by a significantly lower number of veterinarians compared to the first response. The level of association was high (V=0.39, df=3).
The antibiotic therapy selection based on bacteriological testing/AST was answered with ‘occasionally’ (n=23, 39.66%) and ‘always’ (n=17, 29.31%) in significantly higher number of veterinarians compared to ‘frequently’ (n=8, 13.79%) and ‘never’ (n=9, 15.52%). The level of association was high (χ2=55.46, V=0.49, df=3).
The antibiotic therapy selection based on a colleague’s opinion was answered ‘occasionally’ (n=35, 61.40%) in a significantly high number of veterinarians compared to ‘never’ (n=10, 17.54%), ‘frequently’ (n=8, 14.04%), and ‘always’ (n=4, 7.02%). The level of association was high (χ2=55.46, V=0.49, df=3).
The antibiotic therapy selection based on the manufacturer’s manual was answered ‘occasionally’ (n=18, 31.58%) and was non-significantly higher than ‘frequently’ (n=16, 28.07%), ‘always’ (n=15, 26.32%), and ‘never’ (n=8, 14.04%). The level of association was low (χ2=5.31, V=0.15, df=3).
To the question ‘How frequently do you prescribe a combination of antibiotics?’, significantly higher number of answers were ‘occasionally’ (n=43, 75.44%) compared to ‘frequently’ (n=11, 19.30%), ‘never’ (n=2, 3.51%), and ‘always’ (n=1, 1.75%). The level of association was high (V=0.29, df=3).
To the question ‘Do you keep a record of the antibiotics prescribed for the patient?’, significantly higher number of answers were ‘always’ (n=33, 57.89%) compared to ‘occasionally’ (n=11, 19.30%), frequently (n=9, 15.79%), and ‘never’ (n=4, 7.02%). The level of association was high (χ2=46.29, V=0.45, df=3).
To the question ‘How frequently do you weigh patients before giving antibiotics?’, significantly higher number of answers were ‘always’ (n=37, 64.91%) compared to ‘frequently’ (n=10, 17.54%), ‘occasionally’ (n=5, 8.77%), and never (n=5, 8.77%). The level of association was high (χ2=66.13, V=0.54, df=3).
To the question ‘How frequently do empirical antibiotic treatments fail?’, significantly higher number of answers were ‘occasionally’ (n=50, 87.72%), frequently (n=4, 7.02%), and ‘never’ (n=3, 5.26%). There were no answers ‘always’. The level of association was high (V=0.84, df=3).
To the question ‘How often are antibiotic treatments unsuccessful after bacteriological testing and AST?’, a significantly higher number of answers were ‘occasionally’ (n=39, 68.42%) compared to ‘never’ (n=18, 31.58%). There were no answers ‘always’ and ‘frequently’. The level of association was high (V=0.65, df=3).
More detailed description of the response’sdistribution can be found in
Table 3.
 Antibiotic prescribing practices in surgical procedures
Antibiotic prescribing practices in surgical proceduresTo the question ‘How frequently do you prescribe antibiotics after elective surgery?’, significantly higher number of veterinarians have answered ‘>90%’ (n=26, 45.61%) compared to ‘1-10%’ (n=9, 15.79%) and ‘0%’ (n=8, 14.04%), but non-significantly different compared to ’11-50%’ (n=14, 24.56%). The level of association was medium (χ2=19.16, V=0.23, df=3).
To the question ‘On what occasion do you administer antibiotics after surgery?’, significantly higher number of veterinarians have answered ‘When surgeries are contaminated or dirty’ (n=36, 25.35%), ‘When I expect that there will be a leakage from the aseptic area’ (n=32, 22.54%), and ‘Surgeries that last longer than 90 minutes’ (n=23, 16.20%), ‘Prescribing antibiotics after surgery is a common practice’ (n=14, 9.86%), and ‘I have experience with infections after surgery’ (n=11, 7.75%) compared to ‘Depending on the place of living’ (n=1, 0.70%). The level of association was high (χ2=54.42, V=0.23, df=6).
More detailed description on the responses can be found in
Table 4.
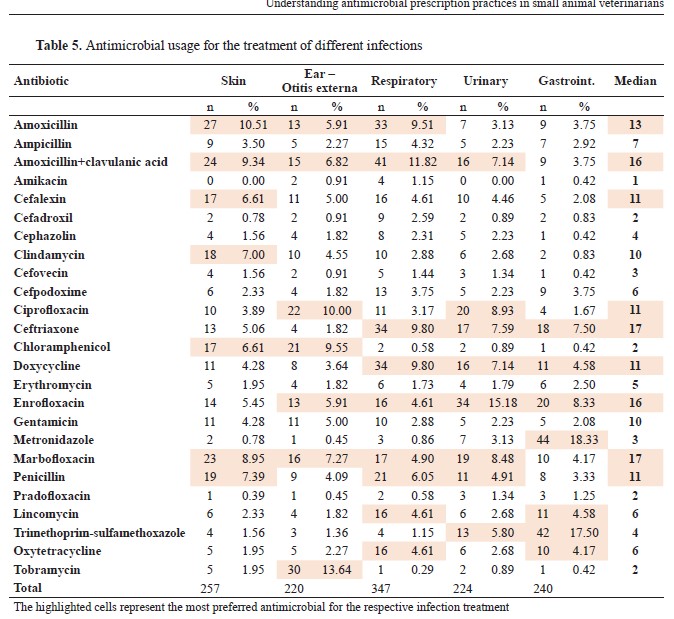
Antimicrobial usage for the treatment of different infectionsFor skin infections treatment, from 257 responses, the most frequently selected antibiotics comprising 56.41% of all responses were amoxicillin (n=27, 10.51%), amoxicillin+clavulanic acid (n=24, 9.34%), marbofloxacin (n=23, 8.95%), penicillin (n=19, 7.39%), clindamycin (n=18, 7.00%), cefalexin (n=17, 6.61%), and chloramphenicol (n=17, 6.61%). For otitis externa treatment, from 220 responses, the most frequently selected antibiotics comprising 59.1% of all responses were tobramycin (n=30, 13.64%), ciprofloxacin (n=22, 10.00%), chloramphenicol (n=21, 9.55%), marbofloxacin (n=16, 7.27%), amoxicillin+clavulanic acid (n=15, 6.82%), amoxicillin (n=13, 5.91%), and enrofloxacin (n=13, 5.91%).
For respiratory symptoms treatment, from 347 responses, the most frequently selected antibiotics comprising 65.71% of all responses were amoxicillin+clavulanic acid (n=41, 11.82%), ceftriaxone (n=34, 9.80%), doxycycline (n=34, 9.80%), amoxicillin (n=33, 9.51%), penicillin (n=21, 6.05%), marbofloxacin (n=17, 4.90%), lincomycin (n=16, 4.61%), and oxytetracycline (n=16, 4.61%).
For urinary infections treatment, from 224 responses, the most frequently selected antibiotics comprising 65.17% of all responses were enrofloxacin (n=34, 15.18%), ciprofloxacin (n=20, 8.93%), marbofloxacin (n=19, 8.48%), ceftriaxone (n=17, 7.59%), doxycycline (n=16, 7.14%), amoxicillin+clavulanic acid (n=16, 7.14%), trimethoprim-sulfamethoxazole (n=13, 5.80%), and penicillin (n=11, 4.91%).

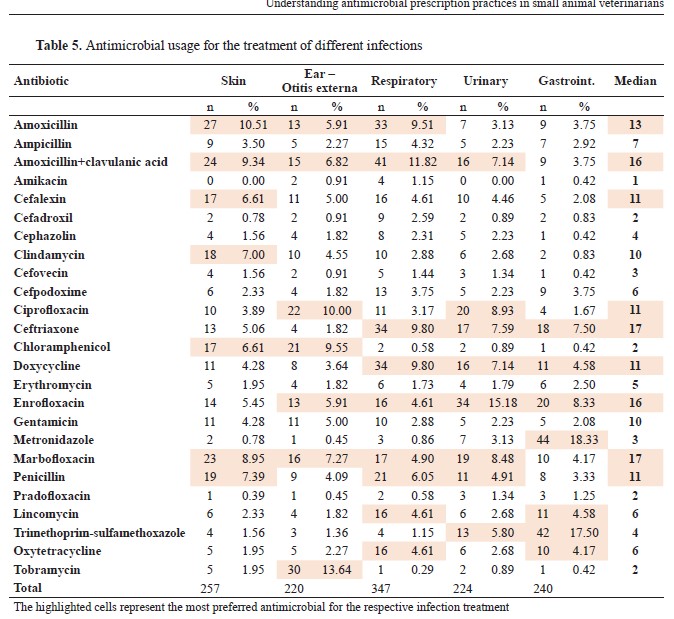
For gastrointestinal infections treatment, from 240 responses, the most frequently selected antibiotics comprising 64.99% of all responses were metronidazole (n=44, 18.33%), trimethoprimsulfamethoxazole (n=42, 17.50%), enrofloxacin (n=20, 8.33%), ceftriaxone (n=18, 7.50%), lincomycin (n=11, 4.58%), doxycycline (n=11, 4.58%), and oxytetracycline (n=10, 4.17%).
According to the median, the most frequently used antibiotics were: ceftriaxone (median 17) for respiratory, urinary, and gastrointestinal infections; marbofloxacin (median 17) for skin, ear, respiratory, and urinary infections; amoxicillin+clavulanic acid (median 16) for skin, ear, respiratory, and urinary infections; enrofloxacin (median 16) for ear, respiratory, urinary, and gastrointestinal infections; amoxicillin (median 13) for skin, ear, and respiratory infections; ciprofloxacin (median 11) for ear and urinary infections; penicillin (median 11) for skin, respiratory, and urinary infections; doxycycline (median 11) for respiratory, urinary, and gastrointestinal infections, and ciprofloxacin (median 11) for ear and urinary infections.
The use of other antibiotics was more selective for treatment of specific infections. Clindamycin (median 10) - skin infections; lincomycin (median 6) - respiratory and gastrointestinal infections; oxytetracycline (median 6) - respiratory and gastrointestinal infections; trimethoprimsulfamethoxazole (median 4) - urinary and gastrointestinal infections; chloramphenicol (median 2) - skin and ear infections; tobramycin (median 2) - ear infections. More detailed description on their use can be found in
Table 5.
DISCUSSIONThis was the first national survey conducted on AMU in companion animals among the small animal veterinarians in North Macedonia. Assessing the current awareness and knowledge of AMU and AMR is crucial as it provides a foundation for achieving success in reducing AMR in companion animals. We observed varying opinions and perceptions among veterinarians regarding the antimicrobial usage patterns. The total response rate of 47.50% is reasonable, given the busy schedules of small animal veterinarians. As seen in prior studies, the online survey format may have resulted in lower response rates (
19, 20). Younger veterinarians were more likely to participate due to the electronic nature of the survey (
19).
Veterinarians considered several factors when choosing antimicrobials for their patients, including their perception of the drug’s effectiveness, ease of administration, and personal preferences and experiences (
4, 21). Our study revealed that “scientific literature” and “own experience” were the two most influential factors affecting veterinarians’ prescribing behavior, with 45.61% and 43.86%, respectively. Experience plays a crucial role in shaping the prescribing behavior of veterinarians (
13, 14). A study on antimicrobial prescribing behavior in Europe (
8) suggests that scientific literature and continued education could be influential factors (
13, 15). It is important to mention that Hughes et al. (
22) conducted a study which revealed that a significant number of practitioners rely on the information provided by the pharmaceutical industry. This may lead to biased information being used in practice due to the promotional influence of this industry (
22).
On the other hand, it has been observed that pet owners significantly influence the prescribing practice of veterinarians (
23). Based on our survey, a significant number of veterinarians (45.61%) answered that pet owners occasionally demand antimicrobial prescriptions, while 35.09% of veterinarians answered that the owners frequently do. Frey et al. (
24) indicate that some pet owners lack awareness of antimicrobial drug side effects and would still want antibiotics for their pets even when the efficacy is uncertain. Moreover, the lack of AMR awareness among pet owners can be a significant obstacle in making decisions regarding the diagnosis and treatment of their pets (
25). Our study further supports this because a large proportion of pet owners either do not seek or only occasionally seek bacteriological testing (38.60% and 59.65%, respectively).
The initial choice of an antibiotic is usually made based on empirical evidence (
1). Veterinarians need to know the different types of bacteria that cause infections in various organ systems, as this helps in the empirical choice of antibiotics (
26). If an infection is causing discomfort or is complex or lifethreatening, antibiotic treatment typically starts before the culture and AST results are received (
26). However, these tests are essential tools for antimicrobial stewardship (
27). It is concerning to use prophylactic or empirical antimicrobial therapy without testing (
28), especially when using fluoroquinolones, macrolides, and third- and fourthgeneration cephalosporins (
29). Our findings show that bacteriological testing/AST is not commonly performed before prescribing antimicrobials, which is consistent with other studies that have reported low AST usage in veterinary practice (
21, 30). A study by Chipangura et al. (
19) reported that 81.22% of patients returned due to ineffective empirical antibiotic therapy. This finding aligns with our results, where a large percentage of veterinarians (87.72%) reported experiencing occasional failure of empirical antibiotic treatment. Moreover, in our study 68.42% reported that even after bacteriological testing and AST, the antibiotic treatment was unsuccessful. Most veterinarians follow the practice of requiring bacteriological testing and AST in cases of recurrent infections like skin (19.63%), urinary (18.40%), and respiratory (14.72%) infections. They also follow the same practice for systemic infections or in cases where empirical therapy has proved to be ineffective.
It has been reported that waiting time for AST results and cost constraints discourage from using these tests (
21, 31). Diagnostic cytology is recommended whenever possible, as it can provide valuable information in identifying the specific microorganisms involved and guide the selection of appropriate antibiotics (
21). A study conducted in Italy revealed that only 5% of antimicrobial prescriptions in a veterinary teaching hospital were supported by the results of microbial culture and antimicrobial susceptibility testing (
32). In our study, 15.52% of the veterinarians rarely or never used bacteriological testing and AST. This lack of confirmed diagnosis can lead to the misuse of antimicrobials, which can have serious consequences (
7, 33).
Beside choosing the appropriate antibiotic, it is crucial to consider the dosage and duration of antimicrobial therapy when prescribing medication (
7). For example, to optimize treatment outcomes in non-complicated urinary infections, it is generally recommended to prescribe a shorter course of antimicrobial therapy, ideally based on AST, lasting between 3 to 5 days (
29). Chronic infections, skin infections (deep pyoderma) and infections with intracellular pathogens often require longer treatment (
26). According to our results, 54.39% of veterinarians preferred a longer 5-10 day-course of antimicrobial therapy, which is consistent with the findings of a study conducted by Zhuo et al. (
34). In contrast, 38.60% preferred a shorter course of 3-5 days while only 3.51% of veterinarians indicated that their preference depended on the diagnosis. Furthermore, it is recommended to weigh patients before administering antibiotics to discourage under dosing and emphasize the importance of accurate dosing (
27). Our survey found that 64.91% of veterinarians complied with this recommendation.
Antimicrobial prophylaxis is a common practice in veterinary surgery, particularly in elective surgeries such as castration/ovariohysterectomy, where the risk of infection is low (
27). Although it is generally advised not to use antimicrobials in clean surgical procedures, our study found that a significant number of veterinarians (45.61%) prescribed antibiotics after such surgeries (
27). The incidence of surgical site infections (SSIs) in small animal surgery is typically 2-5%, and complications can be affected by factors such as wound type, surgery duration and hospitalization (
27). When administered correctly, antimicrobials can diminish the chances of surgical site infections (SSIs) (
35). However, if antimicrobials are not selected appropriately or administered incorrectly, it can lead to an increase in SSI cases and the emergence of antimicrobial-resistant bacteria (
27). It is important to note that prophylactic antibiotics should not be used as a substitute for surgical asepsis and must be used with caution (
27, 36).
Several studies on companion animals have shown significant use of broad-spectrum antimicrobials and a prescription pattern that does not align with current European guidelines (
3, 7). Beta lactams, particularly amoxicillin and amoxicillin combined with clavulanic acid, are widely used as antibiotics for cats and dogs in Denmark, Finland, Italy, Sweden, Norway, and the UK (
22, 37). Our results support the wide use of amoxicillin and amoxicillin-clavulanic in treating various infections such as skin, otitis externa, respiratory, gastrointestinal, and urinary infections. However, it seems there is a lack of awareness among veterinarians regarding the relevant guidelines and their recommendations for first-choice antibiotics. Clindamycin, for example, is often recommended as the drug of first choice for the treatment of skin infections in dogs (
38). Similarly, amoxicillin and trimethoprimsulfamethoxazole are often recommended as first-line antibiotics for the empirical treatment of uncomplicated urinary infections (
30). Based on our results, these antibiotics are less frequently used in practice (7%, 3.13% and 5.80% respectively). In contrast, doxycycline (9.80%) and amoxicillin (9.51%) are more commonly used for the treatment of respiratory tract infections, as they are also recommended as the first choice in the international guidelines for the treatment of respiratory diseases in dogs and cats (
39). It has been found that among the antimicrobials classified as High Priority-CIAs by the WHO, fluoroquinolones and extendedspectrum cephalosporins are the most commonly prescribed in small animal veterinary practices (
9, 33). In our study, enrofloxacin and marbofloxacin are among the most used antibiotics, even though they are categorized in category B, and they should be given after none of the antibiotics of category C or D is effective (
14). Hur et al. (
40) indicate that dogs are prescribed more antimicrobials than cats. Still, cats receive more high-importance-rated antimicrobials, such as cefovecin, a long-acting third-generation cephalosporin (
41). This may be due to the ease of administration and its 14-day activity duration, which is beneficial for practitioners and owners with oral administration (
23). However, of the 57 veterinarians, 48 (84.2%) stated that they do not use cefovecin to treat bacterial infections, probably because it is not licensed in our country (
42). Our study did not differentiate between the use of antibiotics in dogs and cats. As no data is available to differentiate between antibiotic use in dogs and cats, further research is needed to better understand the antimicrobial use in companion animals in North Macedonia.
The findings of our study can help create the first national guidelines for antimicrobial stewardship in companion animals in North Macedonia. It’s crucial to continue the research and surveillance efforts to monitor and understand the prevalence of antimicrobial resistance (AMR) in companion animals, identify emerging resistance patterns, and develop strategies for prevention and treatment. Other factors should also be considered, such as the availability of licensed medicines in our country, national prescribing policies, and regional differences in diseases and antibiotic resistance (14).
CONCLUSIONIn conclusion, the survey highlighted concerns about antibiotic prescribing practices among veterinarians in North Macedonia. The most concerning finding is that bacteriological and antimicrobial susceptibility testing is not commonly used before prescribing antibiotics. This, along with the frequent use of critically important antibiotics for humans in companion animals, significantly elevates the risk of antimicrobial resistance. Educational campaigns for veterinarians and pet owners are crucial to promote responsible antibiotic use and address this One Health issue.
CONFLICT OF INTERESTSThe authors declare that they have no known conflict of interest in the conduction of the current study.
ACKNOWLEDGMENTSThis research was supported by the Faculty of Veterinary Medicine - Skopje.
AUTHORS' CONTRIBUTIONIC conceived the study, developed the questionnaire, and supervised the manuscript’s writing. IS wrote the manuscript, while MN analyzed the data and interpreted the results. AC was involved in hypothesis formulation and manuscript writing. All authors have reviewed and approved the final version of the manuscript.

 10.2478/macvetrev-2024-0020
10.2478/macvetrev-2024-0020