Providing a secure airway management during general anesthesia could be problematic in some medical cases, especially when there is a risk of regurgitation and aspiration of the gastric content due to increased intragastric pressure. The current study aimed to test the applicability of two types of LMA in several animal species and to compare its effectiveness to the endotracheal intubation method in securing sealed airway respiration as an alternative to using endotracheal tubes. The study was conducted in dogs (n=33), cats (n=9), swine (n=9), rabbits (n=5), sheep (n=7) and roe deer (n=1). One or both types of laryngeal masks were used for each animal species: LMA Classic™-cLMA and LMA ProSeal™-PLMA. The assessment of each laryngeal mask was performed by determining the insertion technique, the possibilities of first-attempt insertion and malposition, the compliance with various animal species, ventilation time, cuff pressure, and sealing capacity. The highest LMA size compatility in dogs (23,87±14,30 kg) was size-3 in six and size-4 in forteen subjects; In swine (43,22±12,32 kg), size-4; In rabbits (3,84±0,36 kg) size-1; and in sheep (48,29±4,65 kg) size-3 and size-4. Ventilation time was highest in swine and roe deer (121,11±42,85 min and 300,00 min, respectively) and lowest in cat (28,33±16,96 min). First-attempt LMA insertion success was lowest in rabbits (60%), and highest in sheep and roe deer (100%). Malposition was with highest rate in rabbits (40%) and lowest in cat, sheep and roe deer (0%). Gastric reflux was most frequently observed in sheep (71,4%) and roe deer (100%). The usage of LMA in the veterinary anesthetic practice significantly improves airway management in animals during general anesthesia. The inflated LMA cuff does not prevent its disposition. Therefore, both the drain and respiratory tubes must be fixed. The usage of LMA in rabbits was associated with higher incidence of malposition and other complications. Our findings suggest that LMA designed for humans can be used for airway management in veterinary medicine.
The laryngeal mask (LMA) is a silicon tube which is shaped like an endotracheal tube and on its distal end opens into an elliptical mask, with an inflatable outer cuff. LMA are available in eight sizes (1-6, also in ½ sizes), depending on the body weight of the human’s patient from neonates to adults. LMA are supraglottic airway devices and they are designed to fit in the hypopharynx and cover the supraglottic structures without intruding into the trachea, thus providing an airway seal (
1).
Brain’s description of the classic LMA in the British Journal of Anaesthesia in 1983 was not the first description of a supraglottic airway, but it was, and has still remained a revolution in safe airway management. By the time of the 4th National Audit Project (NAP4), supraglottic airway devices were being used in 56.2% of the human general anesthesia procedures (
2). The first use of LMA Classic in small animals is reported in 1991 by Fujita et al. (
3).
We hypothesized that LMA would be compatible with several animal species and that they would have higher efficiency in securing a tight airway, with minimal risk for aspiration of gastric contents, compared to the endotracheal intubation technique. This assumption was based following reports for the use of LMA with a socalled 'blind-technique', both in human (
4) and animal species (
5,
6). In some animal species, endotracheal intubation can be challenging due to anatomical specificities. For example, the long incisor teeth in rabbits, and the long oral canal in swine can make the endotracheal intubation impractical.
LMA achieves a tighter enclosure of the larynx whilst securing no protrusion in the trachea. This is the reason why these devices are expected to be more practical in animal species. LMA does not cause hemodynamic changes (
7) and requires less or no local anesthetics during insertion (
5), has a lower incidence of causing tracheal lesions, spasms or coughing, and causes lower increments of intraocular pressure. However, LMA has been correlated with human patients' morbidity during general anesthesia (
4,
7).
Next we hypothesized that LMA would efficiently secure gastric content leakage in animal species following reports in humans (
8). The LMA-ProSeal™ type has a built-in drain tube that conveys gastric regurgitated contents without affecting the respiration. This property would be beneficial in animal species that have a higher risk to regurgitation, such as small ruminants. The data from studies in veterinary medicine about LMA in the prevention of aspiration are ambiguous. Reed and Iff (
7) reported that LMA, compared to endotracheal intubation can prevent aspiration of regurgitated content in adult cats but not in kittens. The same report indicates that endotracheal intubation would be more preferable in dogs undergoing abdominal surgery or being positioned in right lateral recumbency (
7). Therefore, the current study aimed to test the applicability of two types of LMA in several animal species and to compare its effectiveness to the endotracheal intubation method in securing sealed airway respiration.
MATERIAL AND METHODS
The experiment was conveyed in six animal species: 1. Dogs (Canis familiaris), mixed breed (n=33); 2. Cats (Felis ilvestricatus) European Shorthair (n=9); 3. Swine (Sus scrophaferus domesticana), Slovak Large White (n=9); 4. Rabbits (Oryctolagus cuniculus), hybrid Hy Plus (n=5); 5. Sheep (Ovis aries), Merino (n=7), and Roe deer (Capreolus capreolus) (n=1). Descriptive statistics for each animal species is shown in
Table 1. The study protocol was approved by a local ethics commission.
A combination of xylazine or medetomidine and butorphanol, diazepam or midazolam was used for premedication. Ketamine or propofol was used for inducing general anesthesia.
DOG: butorphanol 0,1 mg/kg, xylazine 1,0 mg/kg or medetomidine 25,0 μg/kg, midazolam 0,3 mg/kg or diazepam 0,5 mg, ketamine 5,0 mg/kg i.m.; or propofol 4,0-6,0 mg/kg i.v.
CAT: butorphanol 0,4 mg/kg, xylazine 1,5 mg/kg or medetomidine 80,0 μg/kg, midazolam 0,3 mg/kg or diazepam 0,3 mg, ketamine 8,0 mg/kg i.m.
SWINE: xylazine 1,0 mg/kg, midazolam 0,3 mg/kg, ketamine 15,0 mg/kg i.m.
RABBIT: butorphanol 0,1 mg/kg, xylazine 5,0 mg/kg, ketamine 35,0 mg/kg i.m.
SHEEP: atropine 0,025 mg/kg, butorphanol 0,1 mg/kg, xylazine 0,1 mg/kg, midazolam 0,3 mg/kg, ketamine 11,0 mg/kg i.m.
ROE DEAR: atropine 0,025 mg/kg, butorphanol 0,1 mg/kg, xylazine 3,0 mg/kg, midazolam 0,3 mg/kg, ketamine 5,0 mg/kg i.m.

After the induction, the anesthesia in roe dear and in rabbits was maintained by isoflurane, and in other animal species by bolus of propofol (1/3 of calculated dose), or isoflurane.
Before LMA insertion, a lubricant jelly was used without a local anesthetic on the deflated LMA cuff. Following the appropriate placement of LMA, the cuff was inflated up to 40 cm H2O. All animals had active respiration.
The following human-medicine practiced techniques for LMA insertion were assessed: the index finger, the introducer, and the thumb technique. They are unsuitable to use in a veterinary anesthesia for these reasons:
• too long
cavum oris in dogs and swine
• small diameter of
cavum oris in cats, rabbits
and swine
• robust
dentes incisivi in rabbits
• robust
dentes canini in dogs
• sharp
dentes canini in cats and dogs
The correct insertion, positioning, and sealing of the LMA in the hypopharynx was assessed with the following methods:
1. pharyngeal auscultation – presence of snore represented incorrect insertion of LMA
2. chest adspection – movement of the thoracic wall after manual ventilation (when LMA was placed and inflated) represented correct position
3. X-rays – after first insertions of LMA, radiographs of the head and neck were taken to check the correct position in hypopharynx in some animals
4. adspection of the frontal surface of LMA during removal – presence of gastric reflux represented insufficient sealing
5. measurement of LMA cuff pressure - measured by tonometer when used in dogs, cats, swin and sheep
6. modified bubble test – was used to confirm the correct position of the PLMA cuff tip in proximal esophagus and to detect malposition of PLMA
7. insertion of gastric tube into the built-in drain tube of PLMA – the position of the PLMA cuff tip was checked. Smooth insertion of gastric tube represented correct position of PLMA
The LMA was inserted along the longitudinal axis of the oral, pharyngeal and laryngeal axis (
Fig. 1).
 Figure 1.
Figure 1. Insertion of LMA along the longitudinal axis of the oral, pharyngeal and laryngeal axis
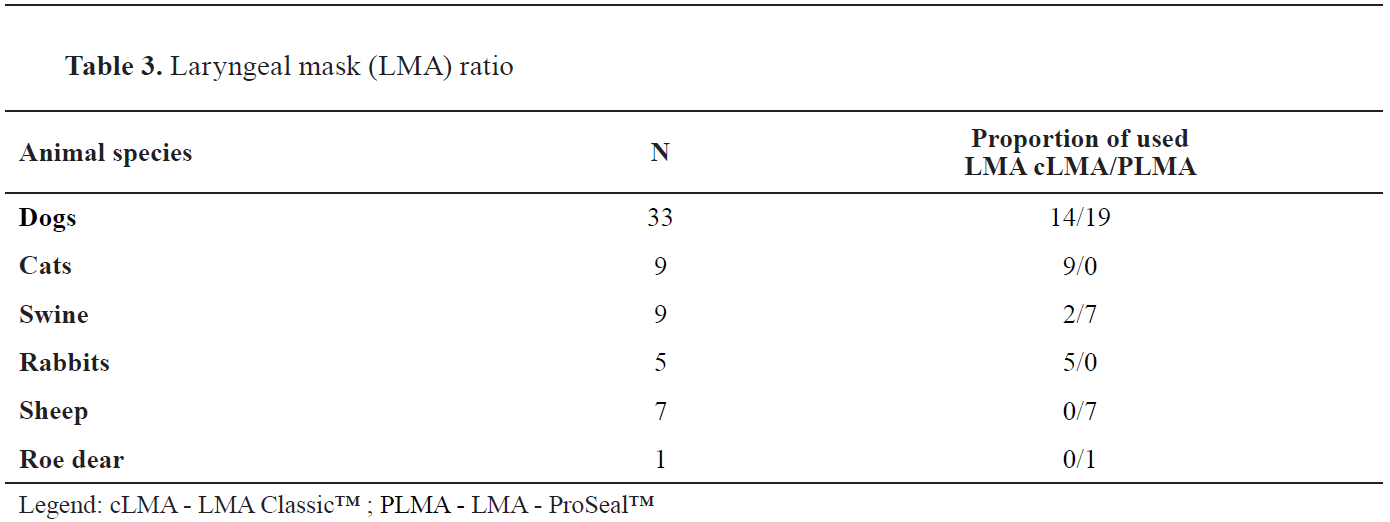
One or both types of laryngeal masks were used for each animal species (
Table 2 and
3) LMA Classic™-cLMA (Teleflex, USA) and LMA ProSeal™-PLMA (Teleflex, USA) (
Fig. 2).
The cLMA is a silicone tube with an elliptical soft silicone cuff. The inflatable outer cuff is connected to a pilot balloon, which is attached to the proximal end of the device. This type of LMA has a standard 15-m breathing circuit connector and an aperture bars designed to prevent the blockage of the airway by the epiglottis (
1).
The PLMA has an additional built-in drain tube next to the airway tube, ending at the tip of the laryngeal mask. This distal tip secures the upper oesophageal sphincter, and when placed correctly, it will cover the opening of the esophagus. PLMA separates the alimentary and respiratory tracts and enables the regurgitated fluid to pass up the drainage tube without leaking into the glottis, therefore reducing the risks of gastric insufflation and pulmonary aspiration. The airway tube of PLMA has shorter length and a smaller diameter compared to the cLMA and has wire reinforcement which, provides flexibility (
1,
8).
The following variables were collected for each LMA use:
• size, size choosing – appropriate LMA size was confirmed by correct positioning and absence of gas leackage
• LMA ventilation time - the time of active respiration trough LMA
• first-attempt LMA insertion - expressed as number of attempts for appropriate positioning of LMA
• malposition – any kind of displacement of the LMA in the hypopharynx
• gastric reflux – was documented as presence of gastric or ruminal content and esophageal regurgitation
• cuff pressure – average inflation volume for achieving appropriate LMA seal, measured for LMA in dogs, cats, swine and sheep
The correct position of LMA cuff in the hypopharynx was checked by X-Ray. The correct position of the distal aperture of the drain tube of PLMA was confirmed by insertion of a gastric tube into the esophagus through the built-in drain tube of PLMA.
 Figure 2.
Figure 2. LMA ProSeal®
RESULTS
Size
Dogs had the highest weight variation from all animal species and were ranging between 3 and 60 kg. Two size-types of LMA were used for body weight range of 15-40 kg for dogs (
Table 4). In 6 dogs we used size-3 and in 14 dogs we used size-4 of LMA.
Initially, small LMA sizes were used for 3 dogs (cLMA-size-2, PLMA-size-1) but were replaced by larger size LMA following the detection of snoring during respiration which was interpreted as inadequate size.
Animals in the swine species group had a body weight of 43,22±12,32 kg. Initially, LMA were selected in sizes of 2, 3, and 4. The first two did not provide an adequate seal on the hypopharyngeal wall and were replaced solely by size-4.
In rabbits, LMA size-1 was used following the recommendations in humans for a bodyweight range of up to 5 kg. In 20% of the animals, dyspnea and/or swallowing reflex was detected soon after inflation. The recommended inflation volume for cLMA of 4 ml was determined to be excessive and was deflated to 2 ml which indicated appropriate positioning.
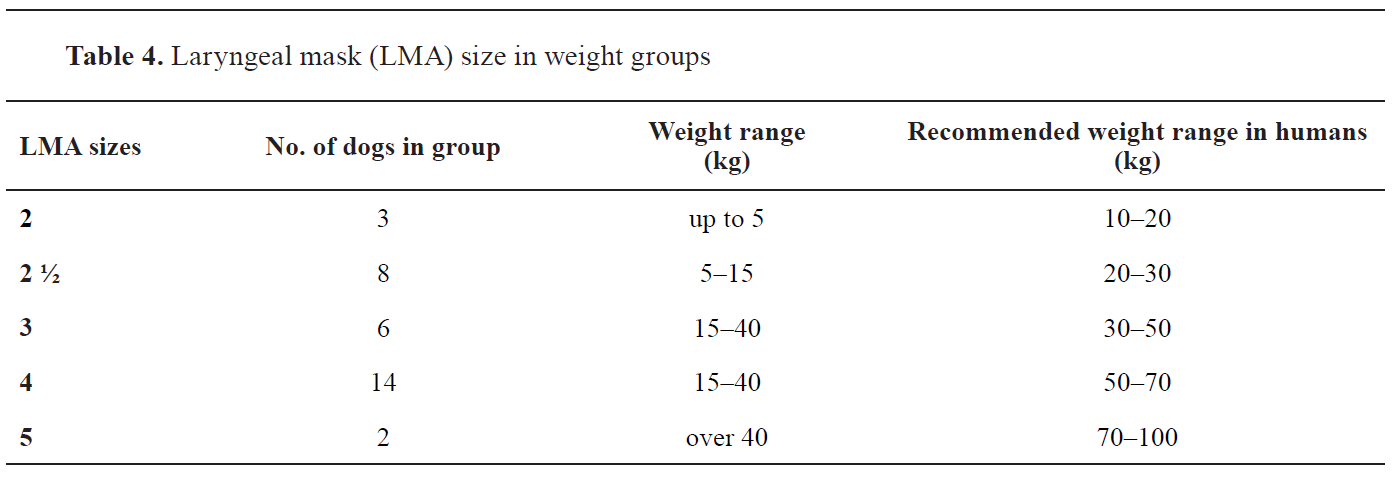
In sheep, PLMA size-3 and size-4 were used. It was observed that size-4 was excessively large for the mean body category (48,29±4,65 kg) due to unsuccessful insertion.
The recommended LMA sizes for humans could not be applied for the animal species included in this research (
table 4). For example, PLMA size-4, which is recommended for human body weight range of 50-70 kg, was compatible in swine with body weight of 43 kg, but incompatible for the similar weight category in sheep (48 kg).
Ventilation time
The longest ventilation time was observed for roe deer undergoing osteosynthesis, and shortest in cats undergoing obstetrics interventions (
Table 5).
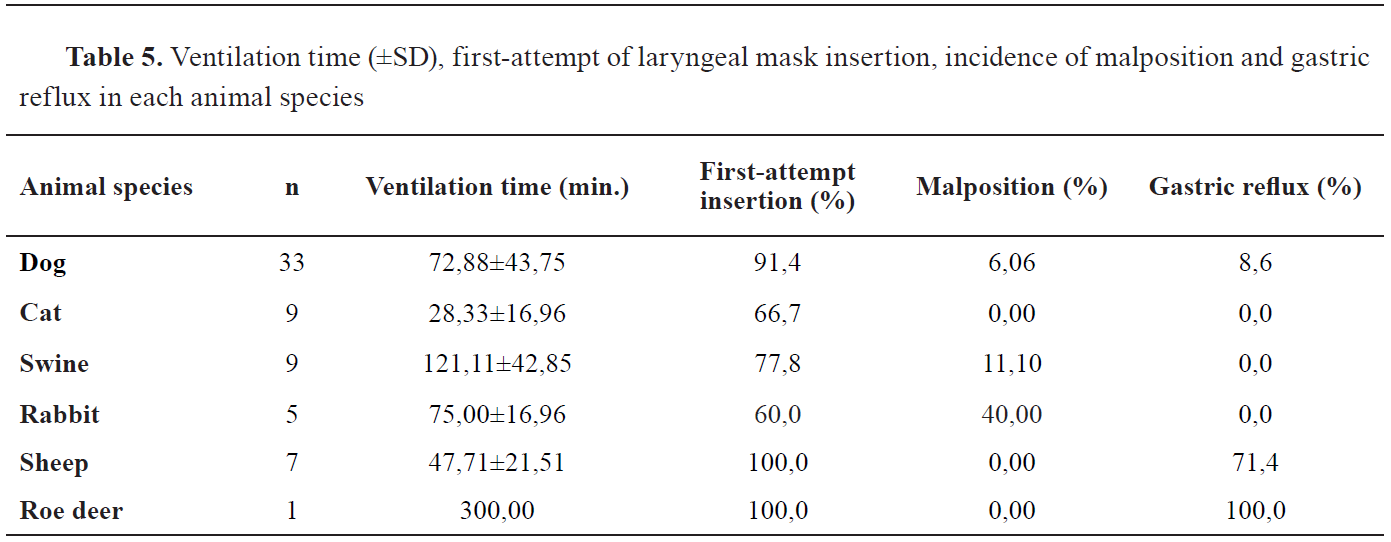 First-attempt LMA insertion success
First-attempt LMA insertion success The lowest success was observed in rabbits (60%) compared to sheep (100%).
Malposition
In dogs, two cases (6,06%) were observed with LMA malposition due to cuff longitudinal rotation following inflation (
Table 5). The most common causes of malposition in dogs were incorrect sizes of the LMA.
In swine, one case (11,11%) was observed with malposition due to twisted gastric probe in esophagus (
Table 5).
In rabbits, two cases (40,00%) were observed with lateral malposition due to longitudinal rotation of the cuff following inflation. Rabbits had highest incidence for this kind of malposition (
Table 5).
In cats, sheep and roe deer no malposition was observed.
Gastric reflux
Regurgitation was observed in two dogs (6,06%) which had PLMA. One of the observed cases in dogs that had regurgitation was assumed to be caused by another procedure (doublecontrast gastrography) since second wasn't food deprived 6-hour prior to the procedure. Despite the observable regurgitation in both cases, no regurgitated content could be found following the extraction of the PLMA. This means that the drain-tube has successfully conveyed the gastric content away from the airways.
The presence of esophageal regurgitation was most frequently observed in small ruminants – 100% in roe dear (in 1 from 1) and 71,4% in sheep (in 10 from 14). Despite the food (12 hour) and water deprivation (6 hours), small ruminants had high incidence of ruminal content regurgitation. In the roe deer, which was the only case of this species, the regurgitation occurred most likely due to undergoing urgent intervention without food or water deprivation.
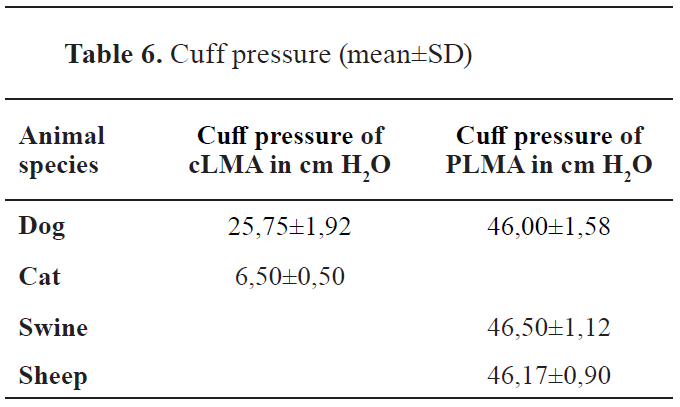
Cuff pressure
Cuff pressure of LMA was measured in dogs, cats, swine and sheep. The average values and standard deviations are presented in
Table 6.
DISCUSSION
Research in human studies reports that PLMA has a lower first-attempt insertion rate than cLMA (
9). Our research in animals did not indicate such a difference.
Our findings indicated that the LMA method requires a lower dosage of propofol compared to the endotracheal intubation method which is in agreement with similar research (
5). Therefore, the risk of cardiovascular depression would be minimized. LMA insertion in dogs was with high first-attempt insertion rate, high tolerance, and low invasiveness.
Wiederstein and Moens (
10) reported that in 63,3% of the dogs included in their study, LMA was successfully inserted, using manual ventilation with inspiratory peak pressures of 10 cm H2O, without any signs of gas leakage. Our findings concurred with this report with an even higher percentage of dogs (90,91%, n=30). Inversely, in Wiederstein and Moens study (
10) higher number of subjects (dogs) had inadequate LMA position and detectable gas leakage compared to our study (63,3% and 9,09%, respectively). Adequate size and positioning of the LMA ensures adequate seal and prevents gas leakage. This can be assessed with the methodology described in this paper. Our findings did not indicate significant differences in LMA insertion among subjects with various body weights. Thereafter, we propose that breed-related differences may not affect the LMA insertion as much as the anatomical specificities of the hypopharynx in each subject.
Asai et al. (
11) reported a higher first-attempt insertion rate of LMA in anesthetized cats compared to endotracheal intubation. In the current study, 66,7% of the cases with cats had successful first-attempt LMA insertion and 33,3% on the second attempt.
Insertion of endotracheal tube is technically a demanding procedure in swine species. Our results show that LMA is an appropriate method for airway control in swine, which is similar to the findings of Wemyss-Holden et al. in 1999 (
12). Their results are indicative that the LMA can be inserted in a simple and fast manner, with a minimal number of complications, even by personnel with low experience in anesthesiology. The LMA designed for humans is compliant with the hypopharynx in swine species. The ventilation can be performed manually with no detectable gas leaks (
12). Fulkerson and Gustafson (
13) have reported concurrently that LMA is much more practical for swine species compared to the endotracheal intubation method.
Reports show easy and successfull insertion of LMA in rabbits during the first attempt, without air leakage in the larynx (
6), inspite of reversible lingual cyanosis in 4 rabbits caused by lingual vascular compression by the LMA. The authors concluded that the LMA is good alternative to endotracheal intubation, because the mask could be inserted easily and rapidly, and its correct placement could be easily confirmed. The current research demonstrated successful LMA insertion in 60% on first and in 40% on the second attempt in rabbits. Furthermore, due to the longitudinal rotation of the cuff and its inflation in the pharynx, we recorded a higher incidence of lateral malposition (40%) and higher occurrence of dyspnea or swallowing reflex (20%) in rabbits. Thereafter, we suggest that LMA could not be considered as an alternative method to the endotracheal intubation in rabbits.
According to Rokamp et al. (
14), the optimized airway seal with cuff pressure lower than 60 cm H
20, and high cuff pressure, may cause paralysis of the recurrent laryngeal, hypoglossal and lingual nerves in human patients. In their study, in 82 patients with a laryngeal mask, cuff pressure was 95 (10 - 121) cm H
2O and above 60 cm H2O which is higher than the recommended level. Out of 56 patients, in 34, the pressure exceeded the upper cuff gauge limit (120 cm H
2O). They did not find any association between cuff pressure and age, BMI, type of surgery, or time from induction of anesthesia to the time the cuff pressure was measured (
14). Sager (
1) reported that following insertion of LMA in animals, sealing could be established by cuff inflation up to the recommended limits (60 H
20) and validated by capnography. In our study average cuff pressure, which provided sufficient cuff seal, was 25,75 cm H20 in dogs and 6,50 cm H
20 in cats for cLMA, and 46,00 cm H20 in dogs, 46,50 cm H
20 in swine, and 46,17 cm H
20 in sheep for PLMA. According to Goldmann et al. (
15), the mean level of airway pressure in swine causing gas leak was 28,80±7,50 cm H
20.
Reed and Iff (
7) has demonstrated that in kittens LMA does not provide protection from aspiration of gastroesophageal reflux. However, in adult cats, LMA reduced gastroesophageal reflux in comparison to a standard endotracheal tube. In cases of prolonged anesthesia during intraabdominal surgery or in cases of right lateral recumbency in dogs, direct endotracheal intubation is more preferable due to a higher incidence of gastroesophageal reflux (
7). Our results differ from the later authors, because of a different model of LMA used in this study. Goldmann et al. (
15) have assessed the positive pressure ventilation in swine by bronchoscopy using LMA-ProSeal™, and have reported signs of aspiration. In their study which included nine animals, the gastric fluid was drained by a gastric tube while no aspiration was detected. This is in agreement with the findings of the current research.
CONCLUSION
The usage of LMA in the veterinary anesthetic practice significantly improves airway management in animals during general anesthesia. Our findings suggest that LMA designed for humans can be used for airway management in veterinary medicine. The inflated LMA cuff does not prevent its disposition. Therefore, both the drain and respiratory tubes must be fixed. We used simple roll bandage to fix the tubes to the maxilla. This prevented the disposition during surgery.
In animal species where intubation must be performed with laryngoscope (swine, rabbits), the LMA can be used with a so-called "blind-insertion" technique. There was a high first-attempt insertion rate of the LMA in almost all subjects in this study. PLMA had prevented aspiration of regurgitated
stomach contents in animal species that have higher incidence of vomiting. The availability of the LMA in various sizes is also beneficial. Adequate size selection for the various animal species could pose a challenge. The usage of LMA in rabbits was associated with higher incidence of malposition and other complications. Thereafter, we conclude that LMA are less suitable for this animal species.
CONFLICT OF INTEREST
The authors declared that they have no potential conflict of interest with respect to the authorship and/or publication of this article.
ACKNOWLEDGEMENTS
Our experimental work has been performed at the Department of Surgery, Orthopedics and Radiology and at the Equine Clinic of University of Veterinary Medicine and Pharmacology in Košice. We would like to acknowledge them for supporting our research.
AUTHORS’ CONTRIBUTIONS
MB proposed the working hypothesis, experimental design of the study, the main investigator, collected data, revision of the manuscript; PV participated on investigation, collected data, processing of the data, draft, and revision of the manuscript. Both authors read and approved the final manuscript.

 10.2478/macvetrev-2020-0020
10.2478/macvetrev-2020-0020